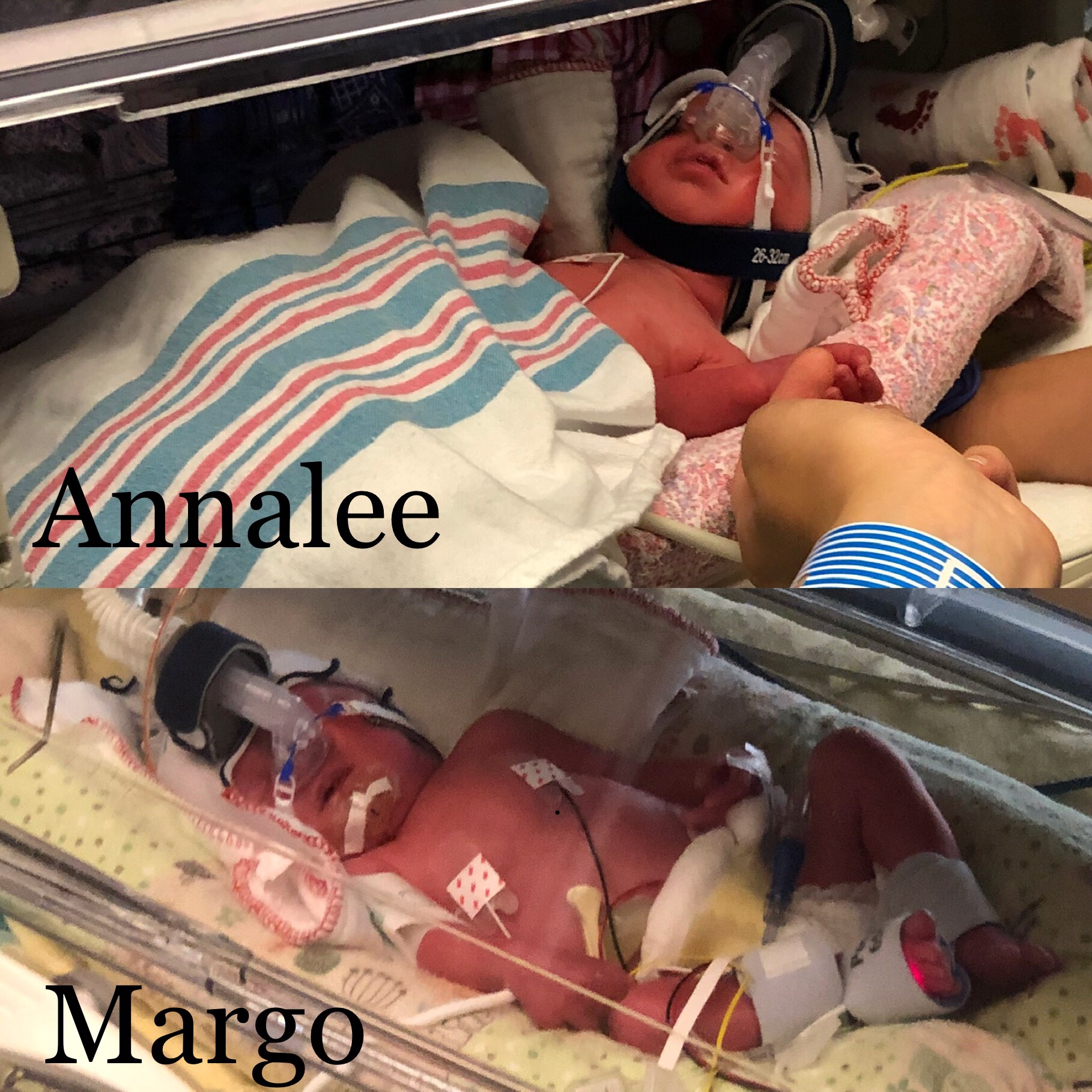
Our baby girls were born on Thursday, September 5 2019 at 1:09 and 1:10 pm
Margo Millie – 3 lb 13 oz
Annalee Mary – 3 lb 11 oz
Some stats:
- 53 days inpatient + 2 days postpartum
- 155 x 1 hour NSTs (these are the heartbeat monitoring sessions)
- 38 separate visitors excluding family!!
- 9 different attending physicians
- More than 16 residents
- 8 entrees on the menu that are actually worth eating
- 5 wristbands
- 4 IVs
- 4 steroid shots (2 rounds of 2)
- 3 art groups
- 3 growth ultrasounds and countless other ultrasounds to find the babies
- 2 false alarms with magnesium drips
- 1 huge dose of gratitude
But let’s back up. Where we left off, we were trying to decide when to deliver the babies. We had originally planned to go to 33w0d, but after a series of false alarms and “we don’t really know what this means” NSTs, we also scheduled ourselves for 32w0d. We had one last ultrasound at 31w5d to help us decide what to do. In the previous ultrasound, the babies were small at 9th percentile and 20th percentile. Since then, I started eating my 2nd breakfast – protein breakfast of champions – to see if I could beef them up. It worked! This time they were 27th and 40th percentile for weight.

We spent days mulling over the decision of when to deliver. We met with the NICU doctors and talked to the OBs. Of course, everyone always wants the babies in longer, but we also knew the decision to wait had risks. They mostly left the decision to us, which implied to me that there wasn’t a strong medical or statistical reason to go either way. It was our choice based on which risks we were comfortable with. Basically, we were evaluating the risks of some short term lung development issues vs the risk of having the babies die in utero. It does happen, and that is why I was in the hospital. In the end, we decided to go with the 32w0d delivery.
The birthday all went pretty well. My c-section was scheduled for noon. I spent the morning packing up the rest of my room, doing crossword-like puzzles, reading Harry Potter, and enjoying the last few moments of being pregnant. Erin arrived a few hours beforehand.

They picked me up from my room and took me straight to the operating room. I was greeted by my doctor and several OB residents who I was familiar with from rounds. It was nice to see familiar faces this time around — so much more relaxed than the emergency c-section with Sam. The worst part of a c-section is the spinal injection. They had me crouch while they did the injection, and I accidentally started laughing at the wrong time. “Not the time to laugh!” Oops. After the spinal, they suddenly ripped some tape off of my back and I yelled “ahh!” Everyone laughed because I am more of a tape wimp than a needle wimp. I was glad I got to lay down after that because the spinal made me feel dizzy due to the scary needle injection and the strange sensation of feeling pressure but no pain. I just tried to focus on breathing.
Once I was all numbed up, they brought Erin in, put up a drape so I couldn’t see, and started cutting away. I could smell burning. “What is that?” The anesthesiologist said “do you really want to know?” It was me—the smell of them cutting with a cauterizer.
After a few minutes, they were ready to pull out the babies. The moment of truth! First out was Margo, yelling and screaming. Then came Annalee, a bit stunned about the whole situation. We decided on the naming order based on how we like saying the names. Margo & Annalee. They were born at 1:09 and 1:10pm.


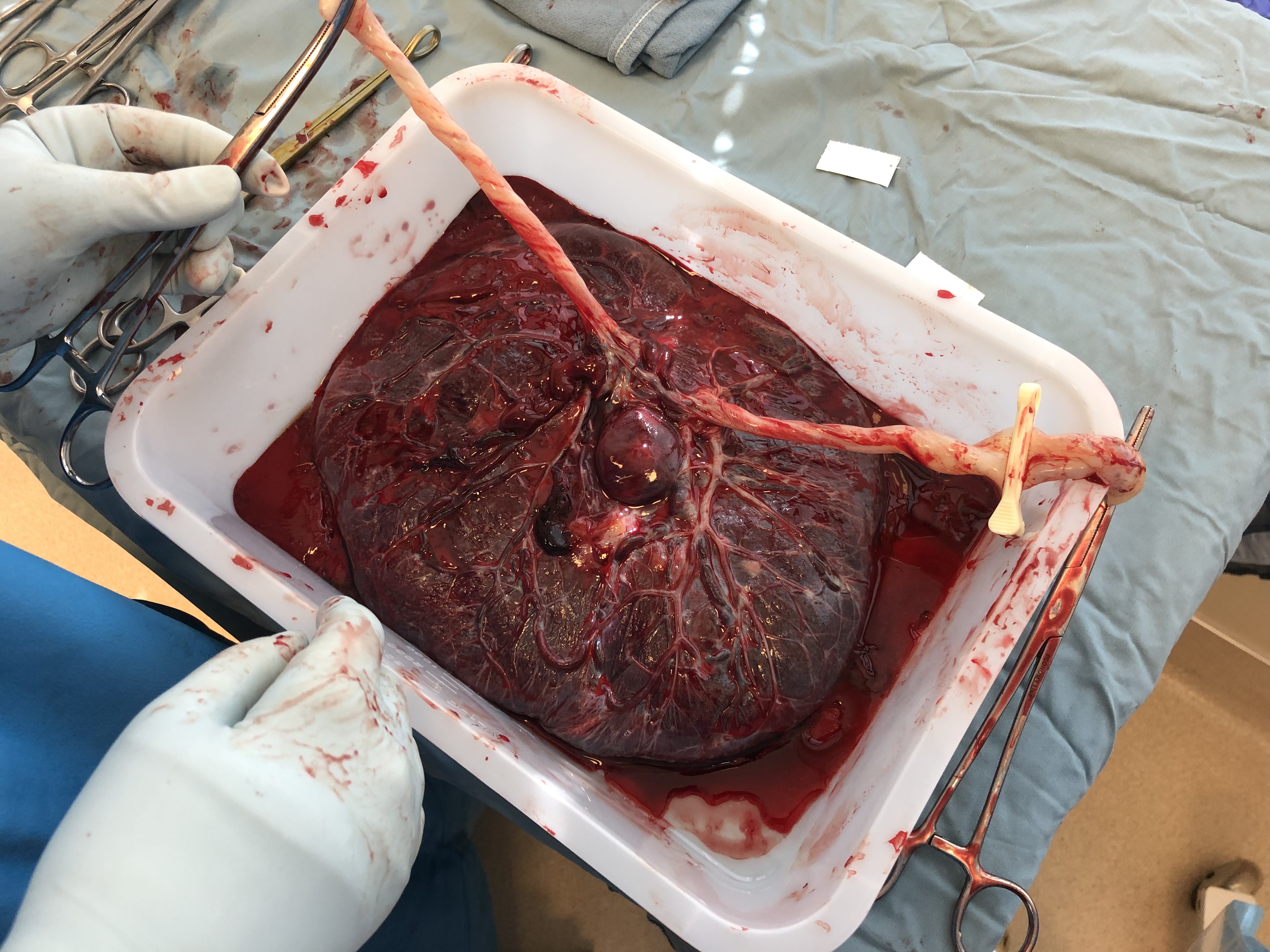
All along, we’ve been wondering what the cords would look like. The majority of momo twins have knots and twists in their cords, and I was so curious to hear/see what ours were like. My doctor said “interesting!” The cords were quite long, with no knots but I think some twists, the insertion points were very close together, and one baby had a cord wrapped around her neck twice. I was a bit bummed that there were no knots! I am guessing it had something to do with how close the insertion points were into the placenta.
Anyway, once the delivery was done, they stitched me back up. That seemed to take forever. Erin went into the room next door where they were stabilizing the babies. I hear that he almost passed out a few times, he helped cut the cords, and other than that I don’t know too much about what went on over there. We counted 15 people in the operating room (including me and Erin) plus probably 8 more in the room next door to help with the babies.

Once the surgery was done, they wheeled me over to labor and delivery for a few hours to recover. At some point we got an update on the babies: Margo was breathing well at birth and didn’t need any surfactant. She got a CPAP right away. Annalee needed a little more breathing help initially so they intubated her, put her on a ventilator, and gave her surfactant. After my recovery period, they wheeled me down to the NICU on a stretcher. By then, Annnalee already had the breathing tube out and was on CPAP.


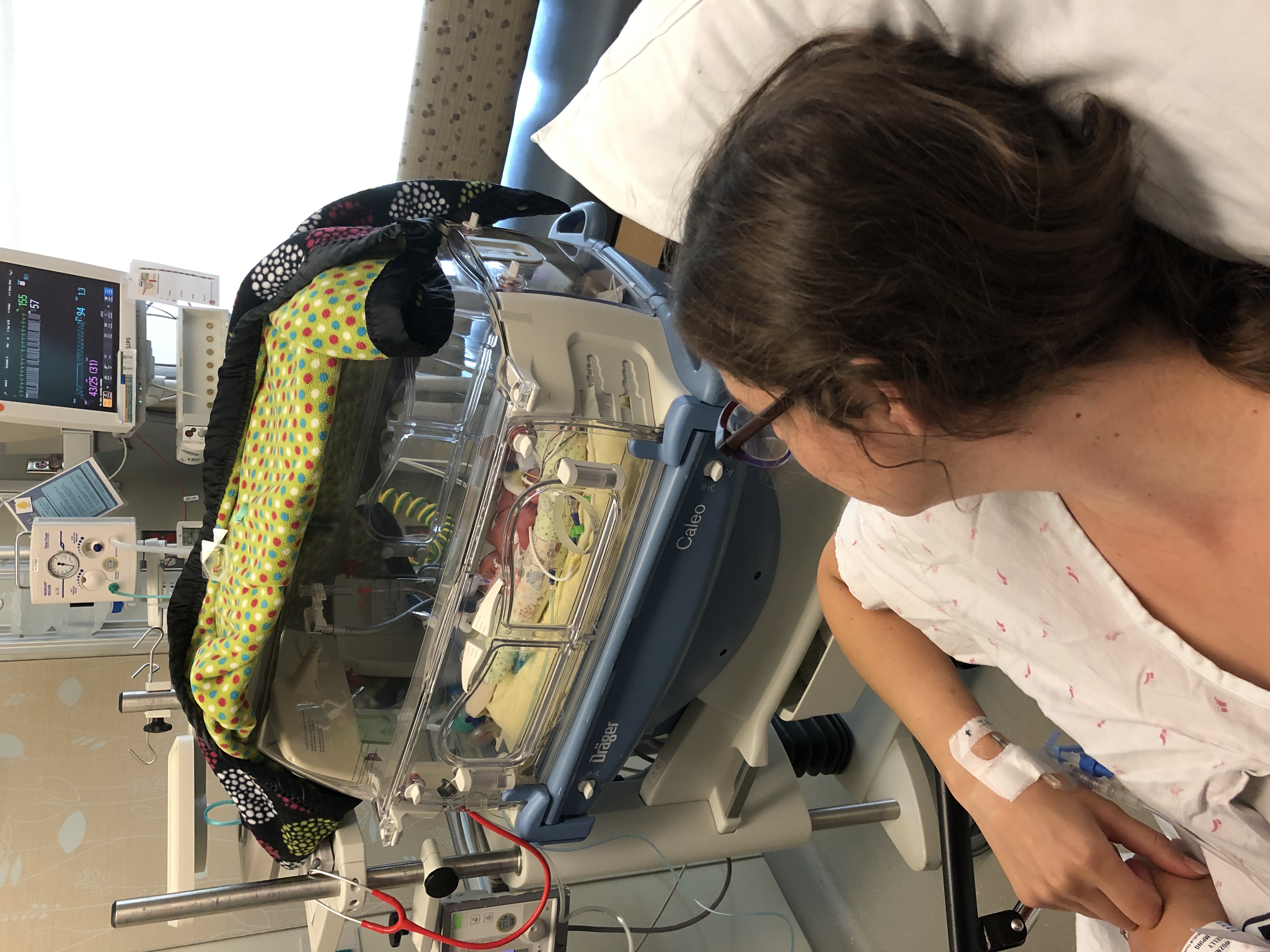

After my short NICU visit, they wheeled me over to the mother and baby unit. It felt somewhat anticlimactic to spend so much time focusing on these babies, and to then have them taken away immediately. It was also strange to be in the mother baby unit alone, without babies or a husband (who went home because why stay?) Now what? I guess I’ll read more Harry Potter.
This c-section was much less painful than the one I had with Sam. I think a few factors contributed to that:
- Last time, they gave me Percocet consistently and only gave me ibuprofen as needed (and they didn’t do a great job of staying on top of it). Times have changed. This time they alternated Tylenol and ibuprofen every 3 hours and only prescribed oxycodone as needed. I only needed one the first night and two the second night.
- Last time, I didn’t get up until sometime on the 2nd day. This time, they made me walk some laps around the mother baby unit the night of surgery. It sucked, but moving sooner than later seems better.
- Last time, the ends of the incision were pulling, and it hurt so much to get up and especially lay back down. This time, the incision must have been a bit better or something because it didn’t hurt nearly as much to get up and down.
Soon after birth, I started the every-3-hours pumping regimen. Otherwise I mostly focused on recovering.
The next day, I got walked down to the NICU to check on the babies. I got to hold Annalee for about an hour or so. I wasn’t able to hold Margo because she was having some breathing sensitivity issues. Those issues continued to worsen throughout the day.

I can’t remember a lot of the details about day 2. I went back to the mother baby unit every 3 hours to get more Ibuprofen/Tylenol, which was annoying. It was a lot of walking for the day after surgery! Erin and Sam came to visit the NICU for a few hours as well.
In the afternoon, Margo’s breathing continued to worsen, so they gave her surfactant to help open up her lungs. Later that night when I was back upstairs in my room, I got a call about how some air had escaped her lung (a pneumothorax, I learned later, which basically means that she got a puncture in her lung and the air went between the lung and chest cavity) and she needed to be put on a ventilator. She also got a chest tube to help get the air out and baby morphine to help with the pain. 😢 Something about the baby morphine broke my heart. Somewhere around this point, the sobbing started, and my surgery pain got much worse — probably from too much walking. I took more pain meds to help with the pain and tried to get some sleep (with of course the every-3-hour pumping wake ups)
When I woke up, it was day 2 after surgery. Time to be discharged. One of the OB residents came by early to talk about discharging me. Meanwhile, I called the NICU to get an update. Margo had a rough night. I just could not stop crying. The mix of emotions, from being inpatient for so long to suddenly being discharged, to feeling guilty for deciding to deliver the babies earlier, to worrying about our sweet Margo, it was a lot to process. Instead of leaving the hospital upon discharge like a normal person, I went straight to the NICU.
When I got to the NICU, the doctors were rounding on Margo. They provided more details. Details about the pneumothorax, chest tube, ventilator, and baby morphine. I still could not stop crying.
We spent a few hours at the NICU that day. I got to hold Annalee again for about an hour, and I helped with some of her diaper changes.
On the way home, we needed to make a stop at Target to get a few things. I felt completely overwhelmed to be back in the outside world. After going through such a long inpatient process, to come home without my babies and to find myself at Target surrounded by tons of people was overwhelming. My first evening at home was full of so many tears. Tears of worry, guilt, some of abandonment after being taken care of for so long. Tears of hormones and being home without my babies. Tears of annoyance that our house is a mess, our dirtbag neighbor started building an extension onto their house that literally touches the fence. Tears of being overwhelmed with the outside world.
As I’m writing this, it is Sunday, day 3, and I am feeling a bit better. Margo had a better day. She did have some additional air escape from her lung overnight, but she has looked good throughout the day. We keep our fingers crossed that she continues to improve. She has been very sensitive to care (her vitals were dropping every time they touched her or even came into the room), but they gave her a PICC line today, which took a few hours, and she did great tolerating that. I know it will still be up and down as she heals — it’s hard to heal a lung when it’s tiny, fragile, and you need it to breathe. But she does seem to be trending in the right direction. Meanwhile, Annalee has been doing quite well. They turned her CPAP down a notch, and she really wants that damn thing off of her face! Both babies are being treated for jaundice.
I know that pneumothoraxes are common, and people always said that the NICU is full of ups and downs. I didn’t really understand what that meant until now. It is so hard to see your little baby struggling, especially given this context where we basically chose to go with the earlier date. I know we made the best decision we could, but it’s hard anyway. I also hadn’t really thought through the psychological impact on the babies of them being in the NICU. It’s better than them not making it out alive, but it makes me sad that they are separated from each other and from me, and that they are going through so much medical treatment at such a young age.
The other surprising thing is how emotional the experience of being discharged has been. A nurse gave me a clue before I left. She said “you’ll be out in the world, and no one will know what you just went through.” So what? Why do people need to know? But it’s true. Especially because my babies aren’t out here with me. I had an amazing team of people checking in on me and taking care of me every single day. It’s hard to suddenly have all those people disappear and to have my routine suddenly change with it. I also worked all through my inpatient experience, so to throw another wrench in the routine change, of course I stopped working now too. I just feel somewhat lost and overwhelmed.
Now it’s Monday as I’m publishing this, and Margo had a good night. No more air escaped her lung, and they are trying to turn the suction off of the chest tube. Fingers crossed that her little lungs have healed.
8 Replies to “55 days later, the babies are here, but our journey is not over”
Comments are closed.